How to Prevent a Needlestick Injury: Everything You Need to Know

Wondering how to prevent a needlestick injury through better sharps disposal and healthcare waste management? The hierarchy of controls implemented to manage and prevent needlestick injuries delivers five key criteria to drive sharps injury risk reduction.1 In its hierarchy of most effective to least effective, the “elimination of hazards” is the most effective control and the adoption of “personal protective equipment” is the least.
Understanding Needlestick Injuries
Occupational exposure to blood and body fluids (BBF) as well as percutaneous injuries from sharps, together pose a serious threat to public health. An estimated 30+ million healthcare workers face a pathogen-exposure risk from a sharps-related occupational injury, which, although preventable, is often regarded as a common workplace injury — a systemic part of the job.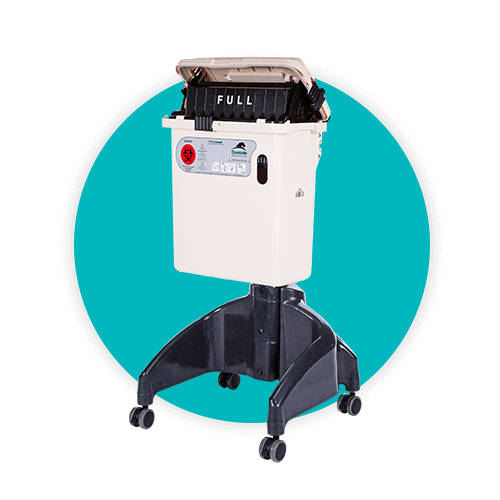
Associated Risks
The World Health Organization (WHO) estimates nine percent of healthcare workers face bloodborne pathogen exposure each year,2 while the Centers for Disease Control and Prevention (CDC) asserts that more than 600,000 sharps-related injuries are incurred by health professionals each year3. There are more than 20 bloodborne pathogens that can be transmitted from contaminated needles or sharps via occupational exposure incidents, including infectious diseases such as hepatitis B (HBV), hepatitis C (HCV), and human immunodeficiency virus (HIV).
Increased workloads and poor organization have contributed to increases in sharps injury risk and close calls for hospital workers.4 Additionally, there is an increasing amount of research tying fatigue and stress to sharps exposure rates.5
In the Event of a Needlestick/Sharps Injury, What Should You Do?
In the event of a needlestick injury, immediate action is essential. So, what should be done first in the event of a sharps injury?
- First, wash the affected area or flush the eyes, nose, or mouth if exposed. Report the incident to a supervisor right away, as quick reporting is critical for effective response. Seek medical evaluation promptly to assess the need for post-exposure prophylaxis (PEP), especially important for potential HIV exposure, which should start within 72 hours. Documentation of the incident should follow OSHA’s guidelines for recording and privacy. For more information about immediate sharps injury management, visit this page.
The Hierarchy of Controls for the Prevention of Needlestick Injury
Reducing needlestick injuries by the greatest amount possible must entail a combination of the following initiatives:
-
Elimination of sharps-dependent procedures
-
Safer devices, including the use of safety-engineered sharps containers
-
Education of healthcare workers and active elimination of risks
SHARPS INJURY CONTROLS RESOURCE
Needlestick Precautions — Elimination of Hazard
When looking to ensure needlestick injury prevention, eliminating hazards from the patient environment is critical. The most effective adopters of this methodology have executed the following changes within their healthcare setting:
-
Use of needleless systems
-
Elimination of unnecessary injections
Engineering Controls
Engineering controls are mechanisms that can positively influence the safety of the sharps deposition and staff contact. The most common controls that drive the greatest impact in sharps injury reduction are:
- Needles that retract, sheathe or blunt immediately after use
- Sharps containers that protect users via hand-access restriction design, letter-drop style of deposition, and inbuilt safety mechanisms
Administrative Controls
Administrative controls are directly impacted by the “exposure environment” and committee/departmental focus; ultimately asking the question of how we will ensure we positively direct and reinforce sharps disposal behaviors across leadership, full time staff, and temporary staff. These include:
- Polices limiting hazard risk and implementing universal precautions around bloodborne pathogen exposure
- Needlestick prevention committee
- Allocation of resources that drive healthcare worker safety
- Training and education around the use of safe devices
Work Practice Controls
Work practice controls are executed “in practice” – to dissect this simply, “when you have a sharps in your hand, what do you do?” The basic safety principles that follow the hierarchy of control are as follows:
- No recapping of needles (Studies reviewing implementation of a “no recapping” policy have shown a 2/3rd reduction in needlestick injuries)
- Place sharps containers at eye-level and at arms reach
- Empty sharps containers before they are full

Personal Protective Equipment (PPE)
This is your basic ‘occupational risk management’ – removing the barriers and filters that exist between the healthcare worker and the hazard to minimize risk.
- Utilize double-gloves to prevent needlestick injury
- Ensure PPE is utilized during procedure
Comprehensive Needlestick Prevention Programs
Ultimately, a needlestick prevention program must look at all facets of sharps injury risk: Adoption of safety-engineered devices, use of safer sharps containers with inbuilt safety mechanisms, critical analysis of the exposure environment and identification of hazards, and the ongoing training and education of healthcare staff in proactively managing sharps injury risk.
To comprehend and drive sharps injury reduction in healthcare facilities, we need to look at a broader safety system that drives protection across the full spectrum of sharps management from the healthcare worker through to the laundry worker who could encounter an incorrectly disposed needle in the laundry.
Daniels Health: Enhancing Needlestick Injury Prevention
Daniels Health plays a vital role in helping healthcare facilities reduce needlestick injuries by facilitating the safe disposal of sharps.
With over 40 years of experience in the healthcare sector, we understand that addressing needlestick injuries requires a multifaceted approach rather than a single solution. Our comprehensive strategy includes adopting safety devices, like our Daniels Sharpsmart container, which boasts unparalleled safety features proven to reduce needlestick injuries by 86.6%, according to a peer-reviewed study.
Sharpsmart — A Sharps Disposal Container With a Difference
This container is designed with hand-restrictive access, overfill protection, and inbuilt security locks, enabling prevention and safety at the point of care.
We also emphasize the importance of education, training, communication, investigation, and engagement in preventing sharps injuries. Our commitment to safety is further demonstrated through providing resources and support for our healthcare partners, aiming to foster a safer working environment and minimize the human cost associated with sharps injuries.
Increasing workloads and poor organization have attributed to two-fold increases in sharps injury risk and near-misses to hospital workers4 together with an increasing amount of research tying fatigue and stress to sharps exposure rates.5
Engage Daniels in Your Proactive Approach
To ensure the highest safety standards and significantly reduce the risk of needlestick injuries within your healthcare facility, it’s time to take proactive steps with Daniels Health.
By partnering with Daniels Health, you’ll not only access our industry-leading sharps disposal systems but also benefit from our extensive experience and resources designed to support your needlestick injury prevention strategies. Don’t wait for another incident to prompt action. Contact Daniels Health today to schedule a demo or consultation and transform your facility’s approach to sharps safety. Together, we can protect our healthcare workers and create a safer working environment for everyone.
Resources to equip your facility in safer sharps management practices:
https://www.cdc.gov/sharpssafety/ | Workbook for Designing, Implementing, and Evaluating a Sharps Injury Prevention Program
https://internationalsafetycenter.org/use-epinet/ | The International Health Care Worker Safety Center at the University of Virginia
https://www.cdc.gov/niosh/topics/bbp/safer/ | Safer Medical Device Implementation in Health Care Facilities
https://www.cdc.gov/niosh/docs/2000-108/ | NIOSH Alert: Preventing Needlestick Injuries in Health Care Settings
References
2Al-Benna S. Needlestick an sharps injuries among theatre care professionals. J Perioper Pract. 2010 Dec;20(12):440-5. PubMed PMID: 21265403.
3https://www.osha.gov/bloodborne-pathogens/quick-reference
4Clarke SP, Rockett JL, Sloane DM, Aiken LH. Organizational climate, staffing, and safety equipment as predictors of needlestick injuries and near-misses in hospital nurses. Am J Infect Control. 2002 Jun;30(4):207-16.
5Clarke SP. Hospital work environments, nurse characteristics, and sharps injuries. Am J Infect Control. 2007 Jun;35(5):302-9.
Let's Talk!
Your time is valuable, and we don’t want to play hard to get. You can either phone us directly on the details listed on our contact page, or feel free to fill out this short form and one of our team members will get back to you as quickly as possible.
