Top Hospital Infection Control Techniques

Understanding how to prevent hospital-associated infections (HAIs) is a key part of overall hospital safety. In fact, infection control in hospitals is at the core of patient safety, staff protection and public trust. Yet despite decades of protocols, training and new technologies, healthcare-associated infections remain a persistent, although often preventable, threat.
According to CDC estimates, roughly one in 31 hospital patients in the United States has at least one healthcare-associated infection on any given day. These infections can lead to extended hospital stays, increased treatment costs, long-term complications and, in some cases, preventable loss of life. In an era of increased public scrutiny, antimicrobial resistance and healthcare worker shortages, the importance of infection control in hospitals has never been more urgent.
Statistics on infection control in hospitals provide promising evidence that demonstrates its effectiveness. Research actually indicates that strong infection prevention programs can significantly reduce HAIs. In fact, the CDC cites studies suggesting targeted prevention steps can decrease specific HAIs by over 70%.
Based on extensive research and first-hand experience, Daniels Health has identified 10 principles of infection control every hospital should prioritize. These steps cover essential infection control techniques, the role of environmental design and practical methods to prevent cross infection through smarter systems and safer waste handling. Whether you’re reevaluating your infection control protocol or looking for new ways to strengthen compliance, these strategies are designed to meet both regulatory standards and real-world challenges.
10 techniques to enhance infection control:
- Build a Facility-Wide Culture of Infection Prevention
- Implement a Clear Infection Control Protocol
- Screen Early, Isolate Swiftly
- Educate and Train Continuously
- Use PPE Based on Risk Level
- Prioritize Hand Hygiene and Environmental Cleaning
- Maintain Proper Ventilation and Airflow Systems
- Ensure Safe Handling and Disposal of Infectious Waste
- Keep Healthcare Workers Vaccinated and Protected
- Audit, Adapt and Improve Continuously
- Stronger Infection Control Starts with Smarter Systems
 Principle 1: Build a Facility-Wide Culture of Infection Prevention
Principle 1: Build a Facility-Wide Culture of Infection Prevention
It’s easy for infection prevention in hospitals to be relegated as the sole responsibility of infection preventionists or environmental services teams. But in reality, it’s a system-wide commitment that touches every role, from intake coordinators and clinical staff to waste handlers and administrative leaders. Building a culture of shared responsibility is the first step in reducing risks and reinforcing compliance.
A strong infection prevention culture begins at the top with leadership. When executive teams prioritize infection control, it’s easier to inspire everyone else to follow suit. In the real world setting of hospitals, this means allocating resources, enforcing accountability and regularly communicating expectations. Cross-departmental collaboration is especially important when it comes to managing workflow overlaps that increase the potential for contamination.
This kind of culture is supported by infrastructure. A well-designed hospital contamination control system ensures safe movement of people, waste, supplies and equipment throughout a facility. Physical layout, cleaning schedules, ventilation and container placement all influence how easily infection can spread or be stopped. It’s all about making safe practices routine, expected and second nature. This requires active engagement across every level of the hospital organization.
 Principle 2: Implement a Clear Infection Control Protocol
Principle 2: Implement a Clear Infection Control Protocol
Every hospital should have a clearly defined, evidence-based infection control protocol that guides staff through both everyday practices and outbreak response. This protocol must be more than a document. It should be a living, operational framework that shapes how risk is identified, addressed, and prevented across departments.
An effective infection control policy outlines how to manage types of infection control responses based on patient risk level, procedure type and exposure potential. It should clearly define when to implement isolation precautions, how to handle suspected or confirmed cases of contagious illness and what roles are responsible for each stage of response.
Strong protocols are built on nationally recognized guidelines for infection control in hospitals, such as those from the CDC, OSHA and WHO. They should also include internal pathways for staff reporting, escalation and incident review. The goal is to minimize confusion and support consistent action, especially when time is critical.
To maintain relevance and compliance, these protocols should be reviewed regularly and updated when new risks or treatments emerge. A strong infection control protocol acts as the backbone of hospital preparedness, prevention and accountability.
 Principle 3: Screen Early, Isolate Swiftly
Principle 3: Screen Early, Isolate Swiftly
Timely identification of infectious risk is one of the most effective ways to reduce transmission and improve patient outcomes. Hospitals that prioritize proactive screening and swift isolation are better positioned to prevent outbreaks and minimize the spread of healthcare-associated infections.
Early screening involves a multi-step process that includes:
- Identifying symptoms
- Obtaining exposure history
- Assessing risk factors as close to the point of admission as possible.
For example, prompt testing for pathogens like Clostridioides difficile, MRSA or respiratory viruses can help staff make informed decisions about room assignment, protective measures and care plans.
Isolation protocols should activate automatically once a high-risk or confirmed case is identified. This includes not only physical separation, but also the immediate deployment of:
- Signage
- PPE
- Containment resources appropriate to the infection type
Clear communication between departments, from admitting and nursing to environmental services, is essential to prevent breakdowns in protocol.
Hospitals that invest in structured triage and isolation workflows are more likely to succeed in preventing hospital-acquired infections, especially in high-volume or high-acuity care environments.
Principle 4: Educate and Train Continuously

Sustained infection control in hospitals depends heavily on the organization’s people. But these staff members won’t automatically know proper protocol. They need training and that training needs to be a continuous process. Ongoing education ensures that every staff member understands how to implement safe practices, respond to emerging risks and prevent lapses in protocol.
Education should go beyond one-time onboarding. Regular training sessions, micro-learning modules and department-specific refreshers keep staff up to date on the basic principles of infection control, which includes:
- Hand hygiene
- Sharps safety
- PPE usage
- Reporting procedures
These sessions should also cover evolving guidance for bloodborne pathogens, multi-drug resistant organisms and novel viruses.
Encourage Infection Preventionists to work alongside department leaders to tailor content based on role, risk level and department-specific exposure. Training should also emphasize the importance of infection control in hospitals not just as a regulatory requirement, but as a professional and ethical responsibility.
Embedding infection control education into the workplace culture equips staff to respond confidently and consistently no matter the scenario.
Principle 5: Use PPE Based on Risk Level
Personal protective equipment (PPE) is one of the most visible and essential infection control techniques in any healthcare setting. But effective use of PPE requires the correct selection, consistent usage and appropriate context-based application.
Gloves, masks, face shields, gowns and respirators should be matched to the level of exposure risk associated with each procedure or patient interaction. For example, standard contact precautions may only require gloves and gowns, while airborne precautions for diseases like tuberculosis or COVID-19 necessitate N95 masks and negative pressure rooms.

Training staff to assess risk and choose the appropriate PPE helps reduce waste, prevent over-reliance and, most importantly, minimize exposure. This approach also supports methods to prevent cross infection, not only between patients, but between staff members as well.
PPE should be easily accessible, stocked consistently and regularly checked for expiration or degradation. If PPE isn’t used properly or is unavailable in high-risk moments, the entire hospital infection control framework becomes vulnerable.
Principle 6: Prioritize Hand Hygiene and Environmental Cleaning
 Hand hygiene remains one of the most effective and universally applicable infection prevention in hospitals. Despite its simplicity, compliance with handwashing protocols continues to be a challenge in many healthcare environments. That’s especially true during busy shifts or in high-acuity areas.
Hand hygiene remains one of the most effective and universally applicable infection prevention in hospitals. Despite its simplicity, compliance with handwashing protocols continues to be a challenge in many healthcare environments. That’s especially true during busy shifts or in high-acuity areas.
Enforcing clear protocols for handwashing and hand sanitizing should include training on when to perform each, proper technique, and reminders at critical points of care. Visual prompts, accessible sinks and dispensers, and ongoing monitoring help embed these behaviors into daily routines.
Environmental cleaning is equally critical. This includes regularly disinfecting high-touch surfaces, patient rooms, equipment, and shared spaces, using approved products and methods. Linen handling and room turnover should follow standardized procedures to prevent recontamination. These practices align with the basic principles of infection control and support a broader, system-level reduction in transmission risk.
Clean hands and clean environments form the frontline defense of any hospital infection control strategy and when consistently applied, they protect both patients and staff from avoidable risks
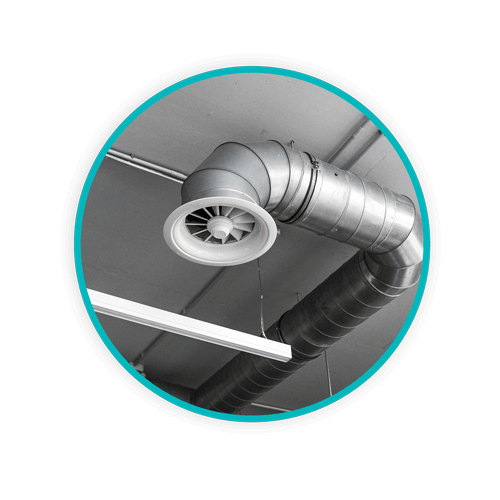
 Principle 7: Maintain Proper Ventilation and Airflow Systems
Principle 7: Maintain Proper Ventilation and Airflow Systems
Airborne pathogens represent a serious transmission risk in healthcare environments, particularly in areas where aerosol-generating procedures are common. Effective ventilation is a core component of a comprehensive hospital contamination control system because it helps to dilute and remove infectious particles before they can spread.
What does proper ventilation look like in a hospital setting? It’s essential to maintain HVAC systems, utilize HEPA filtration, and pressure-controlled rooms (positive for immunocompromised patients, negative for isolation cases). These steps support safer air handling since proper airflow systems play a central role in preventing outbreaks of respiratory infections and reducing the burden of healthcare-associated infections.
During the COVID-19 pandemic, hospitals that invested in ventilation upgrades saw measurable improvements in infection control outcomes. What may have been a pandemic-era concern has proven to be an effective long-term strategy which should be integrated into the infrastructure of every modern hospital.
Regular inspection and testing of ventilation systems is advisable and should be combined with facility design that encourages airflow optimization.
 Principle 8: Ensure Safe Handling and Disposal of Infectious Waste
Principle 8: Ensure Safe Handling and Disposal of Infectious Waste
Medical waste management plays a central role in any infection control protocol, yet it’s often an underemphasized facet compared to clinical interventions. From the moment waste is generated, the risk of exposure begins. And that risk isn’t just reserved to clinicians. Waste poses infection risks to environmental services staff, transport teams, and anyone moving through the facility.
Essential infection control techniques include proper segregation, containment, and disposal of sharps and biohazardous waste. This means using sealed, tamper-proof containers that minimize touchpoints. These containers should prevent overfilling and comply with OSHA and CDC standards. Placement also matters. Containers must be correctly positioned at the point of generation to reduce the chance of accidental exposure.
Daniels Health supports hospitals with clinically engineered solutions that reduce the spread of contamination during use through to their final disposal. Our reusable containment systems are designed to minimize cross-contact, eliminate leakage risk, and improve handling efficiency.
Every touchpoint matters, which is why it’s crucial to choose waste handling systems built with infection prevention in mind. This not only helps protect patients and staff, but also maintains compliance, while reducing risk at scale.
Principle 9: Keep Healthcare Workers Vaccinated and Protected
Because healthcare workers are on the front lines of exposure, they need all of the protection they can get. Without strong protections in place, they can unintentionally become vectors for healthcare-associated infections, putting not only themselves, but their patients and colleagues at risk. No comprehensive infection prevention strategy in hospitals should leave out robust vaccination protocols and staff safety programs.
Vaccination is one of the most effective ways to reduce preventable transmission of viruses such as influenza, hepatitis B, and COVID-19. Having a clear immunization policy aligned with CDC recommendations ensures that staff stay current on required and recommended vaccines.
Beyond vaccinations, staff must be equipped with training, PPE, and resources to respond quickly to exposure events. Post-exposure protocols should be clearly communicated and supported with timely access to care.
Principle 10: Audit, Adapt and Improve Continuously
Even the most thorough infection control protocol can become outdated if it isn’t regularly reviewed. As new threats emerge and standards evolve, hospitals must treat infection prevention as a continuous improvement process.
Schedule routine internal audits to help identify breakdowns in compliance, lapses in training, and inefficiencies in workflow. These assessments should cover every aspect of hospital operations: PPE use, hand hygiene compliance, waste disposal procedures, ventilation performance, and staff vaccination records.
Beyond audits, leadership should actively seek input from frontline staff and infection preventionists to inform changes. Facilities that act on this feedback and make data-driven decisions are better positioned to adapt to shifting risks and implement the most effective methods to prevent cross infection.
Learning from past incidents, as well commending what’s working, supports and encourages smarter planning. It also aligns with best practices for how to improve infection control in hospital environments and strengthens the facility’s overall resilience.
Stronger Infection Control Starts with Smarter Systems
Infection control is a high stakes process for every hospital and it just takes one missed detail to create serious opportunity for harm. By implementing these 10 principles of infection control, hospitals can reduce risk, improve safety, and build lasting trust with patients and staff.
But success doesn’t come from policy alone. It requires the right systems, tools, and partners.
 At Daniels Health, we design clinically engineered waste containment and transport solutions that support real-world infection prevention in hospitals. From minimizing touchpoints to improving placement and disposal workflows, our products and programs reduce exposure risk at every stage of waste handling. We align with the most rigorous guidelines for infection control in hospitals, and help our partners to do the same.
At Daniels Health, we design clinically engineered waste containment and transport solutions that support real-world infection prevention in hospitals. From minimizing touchpoints to improving placement and disposal workflows, our products and programs reduce exposure risk at every stage of waste handling. We align with the most rigorous guidelines for infection control in hospitals, and help our partners to do the same.
Looking to strengthen your hospital infection control strategy? Let’s start with a conversation. Learn about our infection control audits and how we help hospitals improve infection control processes.
Let's Talk!
Your time is valuable, and we don’t want to play hard to get. You can either phone us directly on the details listed on our contact page, or feel free to fill out this short form and one of our team members will get back to you as quickly as possible.
